What is a seizure? A seizure involves random, sudden bursts of electrical activity in the brain. This electrical activity can disrupt brain functions by triggering certain action potentials. However, not all seizures are indicative of epilepsy. In fact, it is possible for a non-epileptic brain to experience a seizure. This likelihood of experiencing a seizure is determined by your seizure threshold. A lower seizure threshold is correlated with epilepsy.
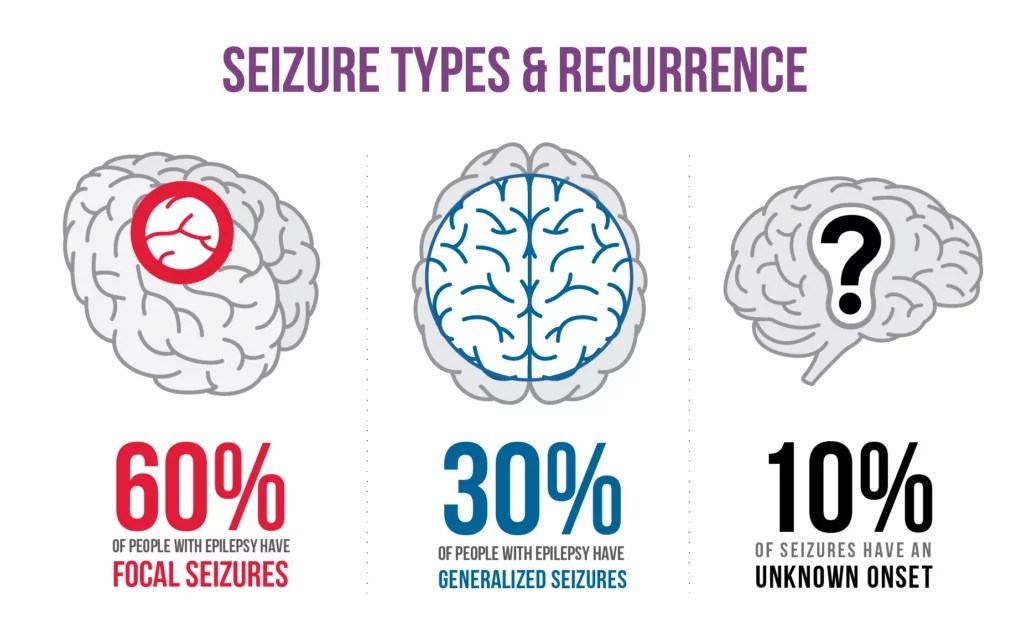
Types of Seizures
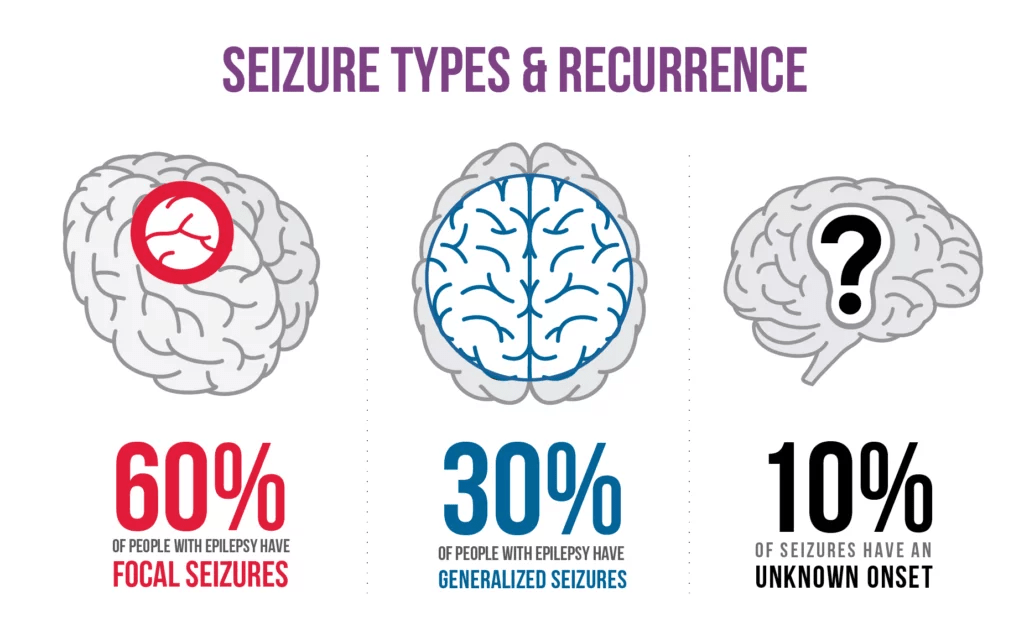
- Focal Onset Seizures: Seizures are called focal onset, when they start from a small groups of cells.
- Generalized Onset Seizures: Seizures are called generalized when they occur on both hemispheres of the brain.
- Unknown Onset Seizures: The origin of these seizures is unknown, hence the name, unknown onset seizures.
Epilepsy
When does a seizure lead to epilepsy? Patients with epilepsy are at a high risk to have recurring and unprovoked seizures. This means that an seizure caused due to withdrawal from drug use, or from a allergic reaction, isn’t considered as epileptic because those seizures would be provoked seizures. On the other hand, a patient with recurring seizures, with no apparent cause, would be considered epileptic.
Cause of Epilepsy
Epilepsy is cause by excessive and abnormal activity in the cerebral cortex of the brain. This activity results in two things. First off, excitatory neurons lose some restriction, allowing them to fire more signals. Secondly, neuron signals begin firing contemporaneously, rather than in order, thus confusing the brain, and the body.
This abnormal activity in the cerebral cortex is caused by phakomatoses, which are a group of diseases that affect the skin and the CNS. One phakomatose that is closely linked with epilepsy in tuberous sclerosis complex (TSC). This disease, caused by mutations in the TSC1, or TSC2 gene, results in increased activity of the mTOR pathway. This activity leads to a growth of tumors in several areas of the body, including the brain. Furthermore, this increased activity in the mTOR pathway causes changes in neural excitability, thus making neurons more prone to fire. This makes it much more likely for an epileptic seizure to occur. In fact, 85% of tuberous sclerosis patients develop epilepsy.
Another phakomatose is the Sturge-Weber Syndrome which is caused by a somatic (relating to the body) mutation in the GNAQ gene. As a result of this mutation, abnormal collections of blood vessels (cerebral vascular malformations) form, changing the flow of blood. 75% Patients with the Sturge-Weber Syndrome also develop epilepsy.
Potential Treatments
- Epilepsy Surgery: Epilepsy surgery is used to treat focal seizures. In this surgery, doctors remove the part of the brain that the seizures originate from. This part is typically a tumor, or malformation.
- Anti-Seizure Drugs: There are two types of medications for epilepsy. The first are Narrow-Spectrum ASMs (Anti Seizure Medications), and are used to treat focal seizures. The second type, Broad spectrum ASMs, can be used to treat a multitude of types of seizures.
- mTOR Inhibitors: These are drugs used to treat epileptic patients with TSC. By inhibiting the activity of the mTOR pathway, neural excitability stays more stable, thus making seizures less likely.
Leave a comment